On this page you will find information and resources about Hirschsprung's Disease.
We have included information about symptoms, diagnosis, treatments, staying in hospital, and more.
The information has been collated from a range of trusted sources, which are linked at the bottom of this page. This page has been written by parents, not medical professionals, so please bear this in mind and always speak to your doctor for medical advice.
Statistics

A note from Georgina
When Ffredi was diagnosed, I googled and googled. I wanted to read as much as I could. I found bits and pieces everywhere but nothing that was comprehensive.
My aim in creating this page was to collect as much information as possible, so when you're ready, you can read as much detail as we know about Hirschsprung's.
What is Hirschsprung's Disease?
Hirschsprung's disease is a rare congenital condition that causes poo to become stuck in the bowels.
Congenital means present from birth.
Normally, the bowel continuously squeezes and relaxes to push poo along, a process controlled by your nervous system.
In Hirschsprung's disease, the nerves that control this movement are missing from a section at the end of the bowel, which means poo can build up and form a blockage.
It is not known why Hirschsprung's disease occurs and there is no way to test for Hirschsprung's disease while you are pregnant. The most accepted theory is that the bowel does not develop ganglion cells in the first 12 weeks of development in the womb.
Ganglion Cells
A ganglion cell is a type of nerve cell. In a person who has Hirschsprung's Disease, the ganglion cells are missing from a part of the bowel. In areas without such cells, the muscle within the bowel wall does not contract to push material through, which results a blockage.
Hirschsprung's disease starts at the rectum. For each person, the amount of colon affected will be different. This can be known as Short Segment (a short piece), Long Segment (a long piece) or Total Colonic (the entire large intestine). For some people, part of their small intestine may be affected also.
The aganglionic portion (without ganglion cells) of the intestine is narrowed and the portion of intestine above this is often stretched from where it has held poo that cannot pass through the rest of the colon. An x-ray can identify a bowel obstruction, but biopsy is the only way to confirm that there are ganglion cells missing from the intestine.
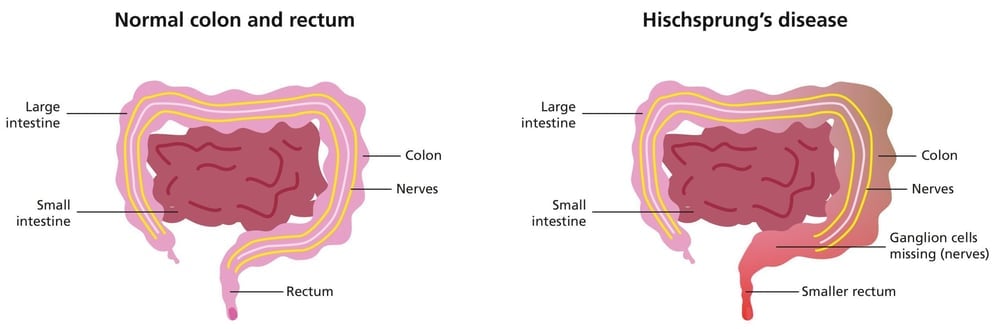
Picture taken from Sheffield Children's NHS Foundation Trust
Symptoms
- Failing to pass meconium within 48 hours. Meconium is the dark, tar-like poo that healthy babies pass soon after being born (although some babies who are later diagnosed with Hirschsprung's disease do pass meconium)
- A swollen abdomen
- Vomiting milky green or yellow-green fluid (bile)
- Reluctance to feed or being slow to feed
Neonatal Admission
Most cases of Hirschsprung's disease are diagnosed during the neonatal period. This is because the main symptom is not passing any meconium in the first 48 hours following birth. Most babies are born at hospitals that do not have paediatric surgical facilities and therefore you may be transferred from one hospital to another.
Children with Hirschsprung's disease are cared for by surgeons. This is because the primary treatment for Hirschsprung's disease is surgery and they tend to be responsible for children with Hirschsprung's before, during and after their surgery and ongoing treatment.

A note from Georgina
One thing we have learned about Hirschsprung's disease is that everyone's experience is very different. Different hospitals treat it slightly differently, every child and their symptoms are different, and every family is different.
So some of this information might not be right for you or applicable. However, if you think something on this page isn't right, please reach out to me and we will review it. If something doesn't feel right about your care, please ask your doctor or request a second opinion.
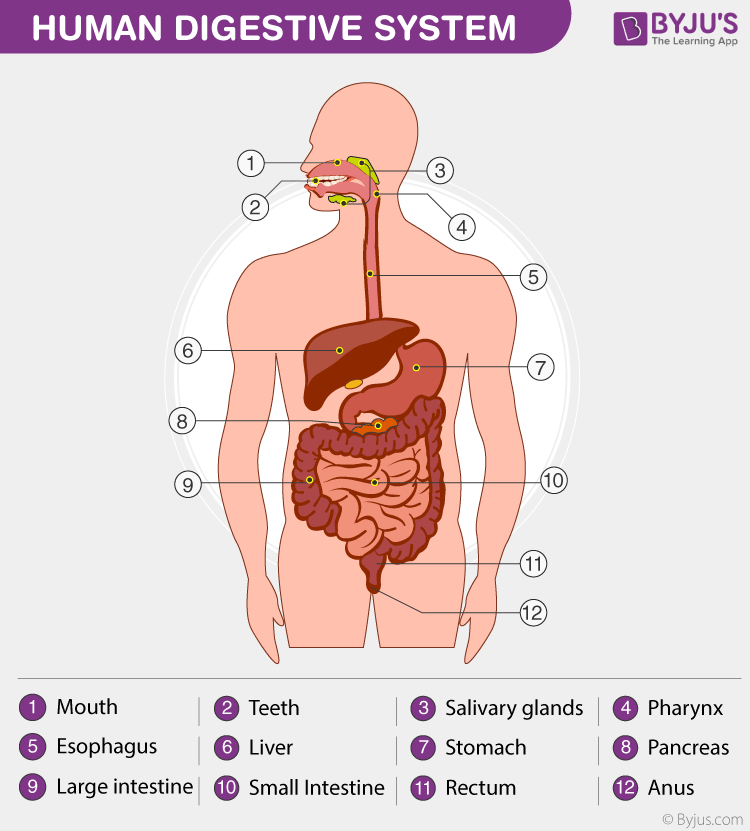
Image taken from BYJUS
The Digestive System
When understanding Hirschsprung's disease, it can be helpful to have an understanding of how the digestive system works.
Your teeth chew food, and saliva (containing enzymes) begins carbohydrate digestion. The food travels down the oesophagus to the stomach via peristalsis (muscle contractions).
The stomach churns food, adds acids and enzymes, and breaks it down into a liquid. The liver, pancreas, and gallbladder also play important roles in digestion by secreting digestive juices and bile.
The small intestine (bowel) absorbs nutrients (proteins, carbohydrates, fats, and vitamins) into the bloodstream.
The large intestine (colon / bowel) absorbs water from undigested matter, forming solid waste (poo).
The poo passes into the rectum which stores the poo until you are ready to release it through the anus.
Co-morbidity
Hirschsprung's disease may occur by itself or in association with other genetic disorders such as Down's syndrome or Waardenburg syndrome. Your doctor will be able to tell you if they suspect any other genetic conditions. For children with Down's Syndrome there is a 40% increased risk of Hirschsprung’s Disease occurring.
Diagnosis
Information taken from Manchester University NHS Foundation Trust
Biopsy
The only definitive way to test for Hirschsprung’s disease is a rectal biopsy – this involves taking a sample of cells from the rectum and looking at them under a microscope.
If Hirschsprung’s disease is present, there will be no ganglion cells in the sample biopsied. A full thickness biopsy is the most conclusive way to test for Hirschsprung's but a suction biopsy may also be used.
Sometimes doctors will do other tests such include blood tests and x-rays. An abdominal x-ray will show a distended (swollen) bowel above the affected section. Sometimes a contrast enema is used to look at the bowel.
Initial Treatment
When a baby presents with the symptoms of Hirschsprung's disease - a swollen tummy and not passing any meconium - it's common for them to begin bowel washouts. This can help stop any poo from sitting in the bowel and causing infection but they may require a stoma if washouts don't work.
Your baby may not take any feeds or be nil-by-mouth and they may be on intravenous fluids through a cannula (tube in their vein) to keep them hydrated.
Doctors may also give antibiotics to prevent and treat any infections.
During this time, your child may also be tested for Hirschsprung's disease.
After Diagnosis
Information taken from Cambridge University Hospitals NHS Foundation Trust
Bowel Washouts
A bowel washout involves inserting a small tube, which is covered in lubricant, up the child's bottom and into their intestine. Warm saline in a syringe is pushed into the intestine. Poo will then flush out through the tube. Your medical team will explain how much saline to use. Sometimes the tube can be removed and re-inserted to encourage the poo to move around. Sometimes a dilator (a steel rod) may be inserted into the rectum to help the saline/poo to pass out of the bottom.
Bowel washouts can be completed daily or multiple times a day before surgery. After surgery, if your child is poorly or is suffering from constipation, you may do bowel washouts.
The resources for bowel washouts (ng tubes or catheters, saline, lubricant, syringes) can be supplied by your GP, local community nursing team or from your hospital. It is helpful to have incontinence or puppy pads to keep mess in one place.
Stoma Surgery
Usually bowel washouts are the first treatment to clear the bowel when Hirschsprung's disease is suspected. If it is difficult to fully flush the poo from the bowel then it's possible your child will have a stoma formed.
A colostomy is a hole in your tummy where a piece of large intestine pokes out. It is sewn in place. An ileostomy is a hole in your tummy where a piece of small intestine pokes out.
Waste will come out of the stoma into a bag that sticks onto your tummy. This waste will look different to regular poo that comes out of your bottom.
Sometimes your child will have two stomas. The second could be a mucus fistula. This is the end of disconnected intestine that goes down to the rectum.
You will learn in hospital how to take care of a stoma and will have support from a stoma nursing team.
Caring for a Stoma
What is a stoma?
A stoma is an opening on to the abdomen (tummy) which allows stool (poo) to flow out. It is formed during surgery.
What does it look like?
Stomas are red, like the inside of your mouth, and are soft and moist. They have a good blood supply, so may bleed a little when they are touched. Stomas have no feeling so it will not hurt.
Colostomy
A colostomy is a stoma that is formed from part of the colon which is also called the large bowel. When poo enters the colon, water is absorbed and the poo becomes drier, it is then passed out of the body via the stoma. The type of poo that comes from a colostomy can either be liquid or more solid in consistency.
Ileostomy
An ileostomy is a stoma that is formed from the ileum, which is part of the small bowel. The ileum is earlier on in the digestive tract and contains digestive enzymes which help to break down food and aids absorption of nutrients from our diet. The type of poo that comes from an ileostomy is generally liquid or pasty in consistency.
Mucus Fistula
In some cases, two stomas can be formed from the same area of the bowel. They are referred to as the stoma and mucous fistula. The stoma is the one that produces the poo, whilst the mucous fistula is said to be non-functioning, but may produce mucous and gas.
Emptying a stoma bag
In hospital you will be shown how to look after your baby’s stoma. One of the first things that you will learn is how to empty the bag. The bag can be emptied into a bowl (this is common in hospital so it can be weighed) or into a nappy. The inside of the pouch does not have to be cleaned once emptied, but it may be beneficial to wipe the end of the pouch to prevent any poo from getting on your baby’s clothing.
When to change the bag
The pouch needs to be changed every 24-72 hours and if it is showing signs of leakage. When changing the pouch, you need to remove the pouch from your abdomen and then clean and dry around the stoma. When applying a new bag, the aim is to fit it snugly around the stoma, so that poo is prevented from going directly onto the skin.
Monitoring
When your child first has the stoma and when you are in the hospital, the nursing staff will make notes on how much poo your child is producing.
They monitor to check that your baby’s output is less in volume than the milk they are receiving. This is important to ensure that your child stays hydrated and receiving nutrition.
Skin Irritation
Although the stoma itself has no sensation, the skin surrounding it does and it can become irritated by both the adhesive on the stoma pouch, and also by the poo itself. Often, these irritations can be minor, but in some cases they can start to cause the skin to break down.
Prolapse and Retraction
A prolapse is when the bowel becomes longer and protrudes through the opening of the stoma. It is not usually serious, as long as the bowel remains pink and active. Retraction of the stoma is when the stoma is below the skin level. This can lead to problems with applying the pouch. You can ask your stoma nurse for help.
Bleeding
The stoma will occasionally bleed, especially when touched; this is normal. However, if the bleeding does not stop or it is coming from inside the stoma then medical advice is required.
Hernias
Hernias are common. Surgery causes a weakness in the abdominal muscle wall allowing parts of the bowel to protrude which creates a bulge under the skin. You can ask your stoma nurse for help.
Bathing
You can bathe your baby with the stoma pouch on or off. Sometimes it is good to allow the skin to breathe.
Clothing
Your baby will not need special clothes, but you should avoid clothes that may rub against the stoma, or prevent the pouch from filling. Similarly, your baby will not need special nappies.
Prescriptions
Normally, your local stoma team will set you up with a prescription delivery service. This could be Respond, Coloplast Charter, Fittleworths or another company.
They will arrange for your stoma supplies to be delivered. You can call them or sometimes order online. You can ask them for samples or try other products.
You should get free dry wipes and bags to dispose of stoma waste. You can contact them if you urgently need supplies.
Products
There are many different stoma products on the market. You can request samples from different companies and you can try different options.
There are a variety of bags, creams and powders that help the skin, rings and paste that help a bag to get a good fit, security strips and more.
Companies include: Coloplast, Hollister, Convatec, Salts, Eakin, Clinimed, Pelican, Cavilon and others.
Pull Through Surgery
A treatment for Hirschsprung's Disease
What is Pull Through Surgery?
Pull Through Surgery is surgery where the piece of intestine that has no ganglion cells is removed and the remaining intestine is pulled down and reconnected to the rectum.
Your child will be put to sleep under general anaesthetic. Firstly, the surgeons will take biopsies from parts of the intestine to work out how much of the bowel is affected by Hirschsprung's disease. Once that has been established, the piece of bowel will be removed. The bowel will then be pulled down and reconnected to the rectum.
For some children, this will happen in one procedure.
For children with a stoma, they will have the pull through surgery first, then a stoma reversal (the surgery to remove the stoma and reconnect the intestine) at a later date to allow the bowel to heal.
For some children without a stoma, a stoma will be formed to allow the reconnected intestine to heal. A stoma reversal will take place at a later date.
For some children, if a pull through surgery can't take place, then a stoma may be formed and the pull through surgery will take place at a later date.
Different Techniques
Pull through surgery can be laparoscopic (keyhole) surgery or open surgery through a larger incision in the abdomen or transanal (through the bottom) or a mix of surgeries. This is down to your individual case and surgeon.
There are different techniques of pull through surgery. You may hear about the Duhamel, Soave and Swenson techniques.
They are named after the surgeons who developed them.
Your surgeon will advise you on the approach they select as well as make the best choice for your child.
After Surgery
Once your child's pull through is done and you have been discharged, they may return to hospital for an examination under anaesthesia where the internal scar will be checked to ensure that it is healing properly. If the scar is tight or narrow, you may do dilations (inserting a lubricated steel rod to stretch the scar tissue to ensure it doesn't cause an obstruction).
If your child has a stoma, you may recycle some of the waste that comes out of their stoma, through their mucous fistula so that the disused intestine and skin begin to become familiar with waste.
After Pull Through Surgery
The Early Days
The first few days after any surgery can be overwhelming. It's likely that your child will be taking pain relief and other medication. It's possible that their bowel may take a short time to recover and they may not want to eat. They will be monitored closely in hospital. Their wound may look very pink and have a small amount of oozing.
After Pull Through surgery, it's likely that children will poo a lot. This can be for days, weeks or months after the surgery. It's also likely that their bottom will be very sore. You may need to apply creams and powders to their skin and do frequent nappy changes. They may be uncomfortable. You should ask for help from your local stoma nursing or tissue viability team as they may have advice on taking care of the skin. Many parents report that the frequency of poo reduces over time. Many children are potty trained normally but for others potty training of faeces may be slightly delayed compared to children that were not born with Hirschsprung’s disease.
Monitoring
Your child's weight may be monitored after surgery to ensure they are gaining weight. Once your child's pull through is done and you have been discharged, they will return to hospital for an examination under anaesthesia where the internal scar will be checked to ensure that it is healing properly. If the scar is tight or narrow, you may do dilations (inserting a lubricated steel rod to stretch the scar tissue to ensure it doesn't cause an obstruction).
Constipation
Some children may struggle with constipation. Laxatives may be given alongside a high fibre diet. If your child is struggling with constipation after pull through surgery, you should see your surgical team. A research study on the outcomes at five to eight years of age for children with Hirschsprung’s disease showed that 50% of children with Hirschsprung's disease did not need any assistance required to maintain voluntary bowel movements. Some children had laxatives and 1 in 5 had bowel washouts to manage their constipation.
Incontinence
Some children struggle with incontinence. This is where a child may poo without intending to. Children with incontinence will receive further treatment and support from their surgical team. A research study on the outcomes at five to eight years of age for children with Hirschsprung’s disease (HD) showed that 57% of children with Hirschsprung's disease experienced some incontinence, half of these children had severe incontinence. In older children and young adults with HD, the proportion who are incontinent of faeces has been reported as ranging from 20% to 50%
Illness
After pull through surgery, it is still possible to get enterocolitis. Many parents report that their children take longer to recover from illness but that as children grow, this reduces and by adulthood no difference to adults without Hirschsprung's disease is reported.
Tests, Procedures, and Complications

Feeding Tubes
When your child is having treatment, they may have a feeding tube. They may have a tube to reduce the likelihood of vomiting or to feed them. Nasogastric (NG) tube feeding involves a tube through the nose into the stomach, they are easy to place and a drainage bag can be attached to the end of it to reduce vomiting. They can be inserted and taken out quickly (and sometimes accidentally). A PEG (Gastrostomy) tube goes through the wall of the child’s abdomen into the stomach, it is placed in surgery. A jejunostomy tube bypasses the stomach dripping feed into the intenstine. Scope

Intravenous (IV) Access
IV cannulation in children involves inserting a small, thin tube (cannula) into a vein to administer fluids, medications, TPN (Total Parenteral Nutrition) or blood. It is commonly used for fluids during treatment or for dehydration. Most commonly a short line is placed, it has a low risk of infection and is easy to place but may not last a long time. Other options include a long line, PICC line and Central line, these may be placed under anaesthesia and are longer lasting.

Blood Tests
For babies, if blood is needed for testing then a small prick can be made on a heel (or when older, finger or toe) and blood can be collected in a pot. Sometimes, blood may be taken by vein.
NHS Greater Glasgow and Clyde

Dehydration
The majority of fluids are absorbed in the large intenstine. This means if a child is missing a large part of their large intestine, they may become dehydrated more quickly than a person who has their whole large intestine. This is more common when a child has an ileostomy. You can support your child by keeping them hydrated with drinks, rehydration sachets and if you think your child needs help, you can seek medical help.

Viruses and other illnesses
Many parents of children with Hirschsprung's disease say their children are more susceptible to viruses and illnesses. They often report that their child takes a longer time to recover than other children. The symptoms of viruses may be similar to that of enterocolitis and if you are worried, you should seek support from a medical professional for reassurance.
Staying at Hosptial
Staying in hospital can be frequent for some families of children with Hirschsprung's disease. It can be a very overwhelming and scary time.
Some children may live far away from their surgical hospital. You may have a consultant at your local hospital and you may have Open Access to the children's ward. This means you don't need to attend A+E to see a doctor, you can ring the children's ward and attend directly.
If you are worried, you can ask your doctor to call your surgical team for advice. You may also wish to attend the surgical hospital directly.
You know your child best and you know how your child presents when they are unwell, if you are in any doubt then please seek medical help.

Where do you sleep?
In the UK, you should be able to sleep alongside your child in the hospital. If your child is in Intensive Care or a High Dependency Unit, you may not be able to sleep alongside your child but may be offered accommodation elsewhere.
Some children's hospitals in the UK have a Ronald McDonald House or Sick Children's House Trust 'Home from Home' locally. Your nurse can refer you for accommodation.
What should I bring?
You can take as much as you like with you to hospital. If you have been attending hospital a lot, you may keep a bag packed at home 'just in case'.
You will always want to pack clothes, pyjamas and you may wish to take toys and things to keep you occupied such as books. For children in nappies or with a stoma, you will want to take your supplies with you.
You may want to take snacks and food as well as things that make it more homely. I always recommend chargers, earphone, moisturiser and lip balm.
Are you entitled to financial support?
Disability Living Allowance
Disability Living Allowance (DLA) for children may help with the extra costs of looking after a child who needs much more looking after than a child of the same age who does not have a disability. Find out more. The amount you are entitled to depends on how much care your child needs, you need to explain in your application what care needs your child has.
Chron's & Colitis UK have a guide on applying for DLA.
Family Fund
If you are the parent of a child with a disability on a low income, you can apply to Family Fund for a range of items. Your child will need support in at least three areas.
Universal Credit
Depending on your earnings, you may be entitled to Universal Credit. The amount of Universal Credit is given based on a number of factors, including if you have a child, if you have a child receiving DLA and if you are caring for the child.
There are Facebook Groups that provide advice for people applying for DLA and those on Universal Credit.
Blue Badge
A blue badge is a parking badge for people with disabilities. Each scheme is run by your local authority. Depending on the disability, you may eligible to receive a blue badge. If your child is under 3, you are entitled if you need to remain close to your car or carry bulky medical equipment.
Carer's Allowance
If you care (more than 35 hours a week) for a child who is entitled to DLA and your earnings are £196 or less a week after deductions, you can apply for Carers Allowance (£83.30 per week). If you are on Universal Credit, claiming Carers Allowance may affect your claim.
You can find out more here.
WaterSure
WaterSure is a scheme to help people who may use extra water due to disabilities. You can apply to the water company that covers your local area. It will place a cap on your water bill so that you are not charged for use over a certain amount.
You can read more here and should apply to your local water company.
Medical Research
There is a lot of research taking place into Hirschsprung's disease in the UK. If you'd like to read more, here's some links to studies and summaries of the research.
Outcomes at five to eight years of age for children with Hirschsprung’s disease
This study reviews outcomes for children with Hirschsprung’s disease who had surgery in the UK and Ireland. It found that while most children survive and do relatively well, many experience significant ongoing problems like bowel and bladder dysfunction, and a notable number need further surgery. The research highlights the importance of long-term follow-up and specialist care to support children and families after initial treatment.
https://adc.bmj.com/content/106/5/484
The patient’s outcome, not the surgeon’s opinion, defines surgical success
This study addresses the need for a comprehensive definition of treatment success beyond traditional clinical metrics. Recognising that measures like readmission rates and length of hospital stay do not fully capture the patient's experience, the researchers developed the Core Surgical Outcome Reporting Treatment Success Score (CSOR TSS). This tool aims to standardize outcome reporting by incorporating both clinical outcomes and patient-reported experiences, facilitating better comparisons across hospitals and enhancing the understanding of long-term quality of life for children undergoing surgery.
https://doi.org/10.1136/archdischild-2024-327768
Hirschsprung's disease in the UK and Ireland: incidence and anomalies
This large, prospective study assessed Hirschsprung’s disease (HD) across the UK and Ireland between 2010 and 2012. It found that the condition affects approximately 1.8 per 10,000 live births, confirming that HD remains a relatively rare but significant congenital disorder.
Boys were much more commonly affected than girls, with a male-to-female ratio of 3.3:1, which is consistent with previous international findings. Importantly, the study revealed that 23% of infants had other associated anomalies, such as congenital heart defects or Down syndrome, and 15% of cases had a recognisable genetic syndrome. This highlights the need for thorough clinical assessment of children diagnosed with Hirschsprung’s disease, as associated anomalies can have implications for both immediate care and long-term outcomes.
Interestingly, the study showed that nearly half of the babies with HD passed meconium within the first 48 hours after birth. Normally, early passage of meconium is considered a reassuring sign in newborns, so this finding suggests that relying solely on meconium passage timing may delay diagnosis. It emphasises the need for greater clinical awareness, as some babies with HD may not present with the classic signs immediately after birth.
In terms of management, 86% of infants initially underwent rectal washouts to decompress the bowel and manage symptoms, but around 27% of these cases eventually needed a stoma due to the failure of washouts. Overall, 36% of all infants ended up having a stoma either as part of their initial management or later on. This shows that while washouts are often effective, they are not successful for everyone, and a significant number of children will require more invasive procedures.
The study ultimately highlights how variable Hirschsprung’s disease can be — both in how it presents and how it responds to treatment — and reinforces the need for early, specialist-led management and long-term follow-up to achieve the best outcomes for affected children.
https://adc.bmj.com/content/109/7/557
Clinical Trials / Studies
There are a range of current clinical trials and ongoing studies into Hirschsprung's disease.
ALOHA
Long-term Qualitative and Quantitative Outcomes of Children With Hirschsprung's Disease and Anorectal Malformations
This study seeks to follow-on from previous studies looking specifically at the long-term outcomes in children with HSCR. Furthermore, the aim is to widen the study to encompass all children treated at Alder Hey and also to use the same methodology to assess long-term outcomes for children with ARMs, as both groups of patients experience similar long term morbidity. This will provide qualitative and quantitative data aiding counselling parents of children with HSCR/ARM.
BEACH
Babies With Enterocolitis - A Study of Faecal Calprotectin in Hirschsprung Disease
In some diseases, a substance called calprotectin is found in the poo when the bowel is inflamed. The investigators plan to collect poo samples from children with Hirschsprung's Disease and measure the calprotectin, to see if it can help the investigators predict which children are at highest risk of enterocolitis.
HAWAII
Hirschsprung's Advances; Working Towards Autologous tIssue therapIes (HAWAII)
Bowel Research UK has begun a new research project aiming to understand the causes and potential treatments for Hirschsprung’s Disease.
This new project aims to understand what stopped those stem cells forming functioning nerves and whether those cells can be ‘switched on’ to grow functioning nerves in the patient retrospectively.
https://www.alderhey.nhs.uk/new-stem-cell-research-project-aims-to-understand-potentially-fatal-newborn-bowel-condition/
https://bowelresearchuk.org/research-hub/development-of-novel-therapies-for-hirschsprungs-disease/
Stem Cell Therapy
A new study led by researchers at UCL and the University of Sheffield, has demonstrated the potential of stem cell therapy to treat those with Hirschsprung disease.
https://www.ucl.ac.uk/news/2024/jun/important-step-forward-stem-cell-therapy-rare-bowel-disease
https://www.sheffield.ac.uk/news/important-step-forward-stem-cell-therapy-rare-bowel-disease
https://gut.bmj.com/content/73/9/1441.info
https://www.gosh.nhs.uk/news/important-step-forward-in-stem-cell-therapy-for-rare-bowel-disease/#:~:text=A%20new%20study%20led%20by,treat%20those%20with%20Hirschsprung%20disease.
Participate in the CSOR Database
The five-year CSOR programme is collecting, analysing and sharing information about how children are currently treated at different hospitals in England and Scotland. The findings will build understanding of how to provide better care and enable hospitals to identify good practice and improve.
If you child has been diagnosed with, or treated for, Hirschsprung's disease, gastroschisis, congenital diaphragmatic hernia, oesophageal atresia, necrotising enterocolitis or posterior urethral valves, AND Was born after the 1st of June 2023, AND Was treated in one of the 10 CSOR hospitals, you can participate.
https://www.npeu.ox.ac.uk/csor/about/how-to-participate